1. Frequency (going to the toilet a lot)
2. Urgency (needing to rush to the toilet)
3. Nocturia (getting up at night to go to the toilet)
It's also common to have pain with intercourse because the bladder is painful and pressing on it during intercourse causes pain.
Some women have times when their bladder is especially bad and they think they have a urine infection. If the urine is collected, often there is no infection found. Just a bit of blood in the urine.
This problem if often due to a condition called Interstitial Cystitis. If you have this problem, there is lots that can be done. We would love to hear your story.



Hi Susan,
ReplyDeleteCan you explain the condition "Interstitial Cystitis", how you can test for it, and some of the ways in which it can be treated?
Dear Tricia,
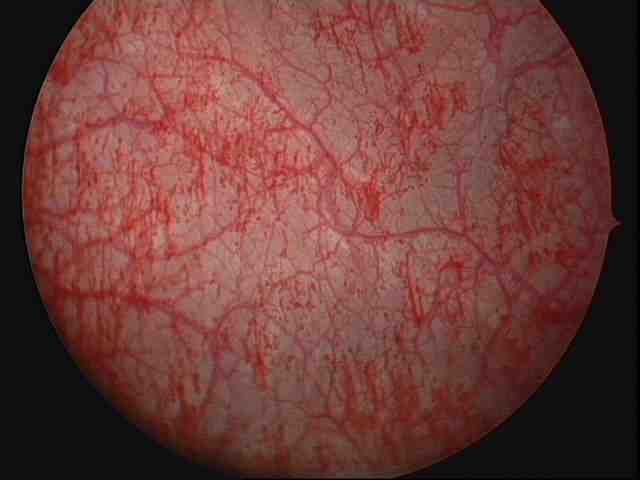
ReplyDeleteCertainly. There is no perfect test for interstitial cystitis, but the best one at the moment is a procedure called a 'cystoscopy and hydrodistension'. A cystoscopy means putting a telescope inside the bladder to look at the inside surface of the bladder. This is usually normal. However, if the bladder is filled up quite full with water at the cystoscopy, and then watched while the bladder is slowly emptied, lots of tiny bleeding points can be seen. The tiny areas that bleed are called 'bleeding glomerulations' and filling the bladder up very full like this is called a 'hydrodistension'.
A normal cystoscopy can be done while you are awake, but a cystoscopy with hydrodistension needs to be done under an anaesthetic as it would be painful if you were awake. If bleeding glomerulations are seen, then you probably have interstitial cystitis. If not, then you have a painful bladder for another reason.
Sometimes the doctor takes a small biopsy (sample) from the wall of the bladder at the same time.
There is still a lot more to be known about interstitial cystitis and bladder symptoms.
Best Regards
Susan
Have stage IV endo with a bladder pain that has increased greatly with superovulation cycles. Had a regular cystoscopy that looked normal but am still having significant pain. Doctor has prescribed prosed ds which seems to help. Have pain after voiding which is helped by drinking a lot of water. I'm also very uncomfortable with a full bladder and I can't tolerate it for very long.
ReplyDeleteDear M,
ReplyDeleteThanks for contacting me. It sounds like you probably have interstitial cystitis. This is an inflammed bladder which causes a lot of pain. It looks normal at a normal cystoscopy. However if you fill the bladder quite full with water while under anaesthetic, then watch the bladder while it deflates, there are many little bleeding points that show up. These are called bleeding glomerulations.
The sort of symptoms that fit with this diagnosis include:
1. Getting up at night more to go to the toilet
2. Needing to go to the toilet more often
3. Needing to rush to the toilet
4. Feeling like you have a urine infection but the urine test just shows some blood, no infection
5. Painful intercourse.
You can treat the problem with a mix of things:
1. Diet changes. There may be a few things that make your pain much worse
2. Medications. Amitriptyline in low dose is a good way to start. If it makes you to sleepy, then ditropan or solifenacin are often helpful
3. Other treatments.
There is more info at www.ic-network.com
If you have flares of pain, then drinking a lot of water often helps, especially if you take a teaspoon of bicarb soda with it, or something like ural which makes the urine less acid.
You may find that a lot of the pain you felt was your endo, is actually your bladder.
I would also say that many women with this, also have tight pelvic floor muscles which can cause pain, especially with tampons or intercourse, or smear tests.
Best wishes,
Susan Evans
Dear M,
ReplyDeleteI have added 2 pictures below to show you what interstitial cystitis looks like. The bottom picture shows what a bladder looks like at normal cystoscopy. The top picture shows the same picture after hydrodistension (filling while asleep and watching as it deflates. It looks sore and it is sore! A normal bladder doesn't have these bleeding points after filling this way.
The list of diet treatments can be found on the IC-network site or our book.
Best wishes,
Susan Evans
Hi Susan
ReplyDeleteI have endo and had it removed 7 years ago from my left ovary and bladder. I assume I have scare tissue on both places as they both still cause me grief. 2 weeks ago i had a miscarriage and had a curettage. For 2 days after the curettage I was feeling fine, however, then developed extremely bad pains in the area on top of my public bone towards the end of urination. It hasn't seemed to have gone away and is very painful. Is it possible the curettage bruised the already sensitive area or could it be possible I have Interstitial Cystitis?
Thanks for your blog.
O.
Dear O,
ReplyDeleteI am sorry to hear about your miscarriage. It is always a difficult time.
Regarding your pains, they certainly could be interstitial cystitis, especially if your bladder was badly behaved before your curettage. By badly behaved, I mean a need to go to the toilet more than your friends, get up at night frequently, or have to rush to the toilet.
Other possible causes include some irritation to the urethra if your doctor used a catheter at the curettage. This usually settles in a few day. Or, a urine infection which your doctor could check for with a urine sample. If the sample shows blood but no infection, that can sometimes mean interstitial cystitis too.
Best wishes,
Susan Evans
doc my wife facing same problem and she was prescribed gonablok 100 plz give me some sugsstion my id
ReplyDeletebanerjeealbert.pord@gmail.com
Dear Sir,
ReplyDeleteGonablok is a brand name for a medication called Danazol. Danazol can make periods less painful, and lighter, but unfortunately it doesn't help pain from the bladder.
Its tricky because both period pain and bladder pain are often felt in the same place (lower abdomen in the centre). Also, women with this often also have painful pelvic floor muscles (tampons, sex and smear tests become painful).
100mg daily is a low dose of danazol, which most women can take without any troubles. It doesn't get rid of endometriosis but it can keep it quiet and usually makes periods lighter.
I find that most women are much better with a mix of:
* Finding and cutting out dietary triggers for IC
* Using a medication such as amitriptyline in low dose, oxybutinin (maybe as patches)
* Managing flare ups with increased water intake and something to make the urine less acid.
If this is not enough there are other more complex treatments.
There are lots of different treatments for Interstitial Cystitis so it is a bit difficult to explain on a blog. However our book has a chapter on the different treatments, with all the information you need to take to your doctor so they know how to help you. It also has information on Danazol and all the other pains your wife probably has too. Its available from our website www.drsusanevans.com.
Alternatively, there is also information at www.ic-network.com
I hope that helps, Best wishes, Susan
hi
ReplyDeleteMadam i m a 30 years old unmarried girl. since last 15 years i m hving severe acute pain in left lower abdomen.i got myself treated in india,s best hospital. All my reports r normal. now i m being treated again. my doctor advised me 2 take gonablok capsules 4 6 months.
while taking these medicine, menstrual cycle stopped and there was no pain. meanwhile i did intercourse. i hve stopped taking this capsule now as 6 months over since last 15 days. but cycle dint start till now. May i be pregnant? or its a normal process.i m woried. please do let me knw whats d problm wid me?????
thanks
Dear Manni,
ReplyDeleteI can see that this would be very confusing for you.
Gonablok is another name for danazol. When you are on danazol, periods usually stop, but it isn't always a reliable contraceptive.
Often it takes a little time for periods to come back after your stop danazol, so you are probably not pregnant, but its worthwhile checking. I suggest that you:
1. Do a urine pregnancy test to make sure that you are not pregnant
2. Start an oral contraceptive pill. This can help stop the pain returning and help you avoid pregnancy in the future.
When you use the pill, its good to have a period only every 2-3 months so that you have less periods and less period pain. Your doctor can explain how to do this.
very best wishes,
Susan
I had twice unsuccessful IUI and now my doctor adviced me 2 months course of gonablok and then do IUI.what is the role of this medicine i?does it improve the success rate of IUI?
ReplyDeleteDear Anonymous,
ReplyDeleteI am sorry to hear that your IUI has been unsuccessful. It is difficult for me to comment on your care as I do not know all the details of your situation. However, I will do my best to answer your question.
Gonablok is another name for a medication called danazol.
Danazol (gonablok) is sometimes used to make periods lighter or less painful. However, unfortunately danazol does not improve fertility.
It makes endometriosis less active while you are taking it, but does not remove endometriosis.This means that when you stop the danazol, periods often become painful again within 6 months.
It is important not to become pregnant while you are using danazol, as danazol can cause abnormalities in a baby.
I hope that this is useful, and wish you all the best for your fertility,
Susan Evans
I have been using gonablok for the past two months but my periods did not stop but came earlier than expected.that is after i started taking them, periods came after 3 days.and the pain is still on. what could be the problem?
ReplyDeleteDear Anonymous, It depends on how much gonablok you are taking. A dose of 100 or 200mg each day for 2 months should make periods lighter but not stop them. A dose of 600 to 800mg each day usually stops periods. Gonablok is a medication called Danazol. It does not improve fertility but can sometimes make periods less painful.
ReplyDeleteIs your pain just with periods, or is it at other times too? Most of the women I see have a few different types of pain. Gonablok will not help pain from pelvic muscles, the bladder, bowel, or pelvic nerves.